Pelvic Floor Exercises for Painful Intercourse
Pelvic Floor Pain During or After Sex
There are all kinds of pelvic pain in the world of pelvic floor physical therapy. And no, I’m not talking about the common (but definitely not normal) period cramping kind of pain. It’s been a minute since I’ve written about pelvic floor issues, but I felt that this was important to discuss.
I’m talking about vaginismus and dyspareunia. You may have heard about these physically and emotionally painful conditions, but not everyone is aware that there are actual names for what they’re experiencing in and around their pelvis. I want to get slightly more specific and perhaps introduce you to two very real sexual dysfunctions that exist in the population that has vulva and a vagina. As an educator, it’s a huge goal of mine to spread awareness of their existence, as well as shed light on things you can do to address them. So here we go.
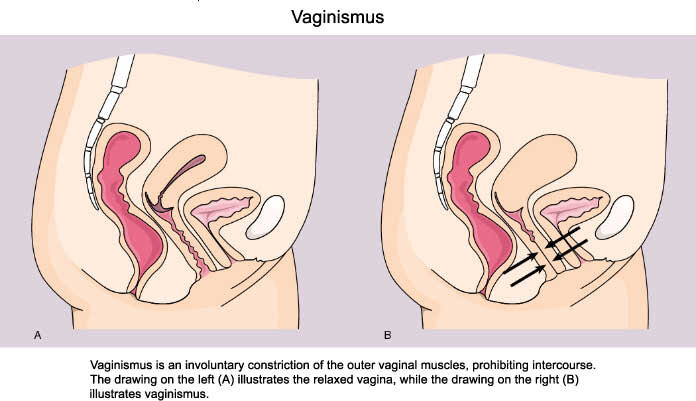
What Is Vaginismus?
Vaginismus is defined as “the persistent or recurrent difficulties of the woman to allow vaginal entry of a penis, finger, and or any object, despite the woman’s expressed wish to do so” (1). My first interaction with someone who had this dysfunction was my lab partner in my first pelvic floor continuing education course. I had no idea this even existed, and she mentioned doing better in her own physical therapy sessions, since she was able to accommodate a prodding finger for an assessment. She had just started using tampons in her mid-twenties.
People with vaginismus may actually avoid intercourse, pelvic exams, and the use of insertable menstrual products due to the hyperactive muscular tissue that reflexively spasm in response to anticipatory fear, anxiety and pain. Although, “it appears that vulvar pain and the fear of pain or of vaginal penetration characterizes most women currently diagnosed with vaginismus” (2).
A course I took called Sexual Medicine in Pelvic Rehabilitation related this condition to prevalence in certain cultures, which blew my mind. Women are unable to consummate their marriages due to primary vaginismus (they’ve never been able to tolerate penetration) versus secondary vaginismus (they may have tolerated penetration, but now experience a “pushing out” sensation). These women may have “excessive closeness of family members, allowing the family to be intrusive and exercising pressure on the couple, a strict education which highly values virginity, transmits fear of ’the male’ and fear of sex, linking sex with pain.” (3).
This actually reminded me a lot of conversations I’ve had with friends who grew up in religious households like myself, which undoubtedly impacted their relationships with significant others and their relationships to their sexuality. It’s one of my favorite topics of conversation, honestly, and I look forward to leading more conversations on this topic in future courses, classes, and workshops.
Now, how do we differentiate vaginismus from dyspareunia?
What Is Dyspareunia?
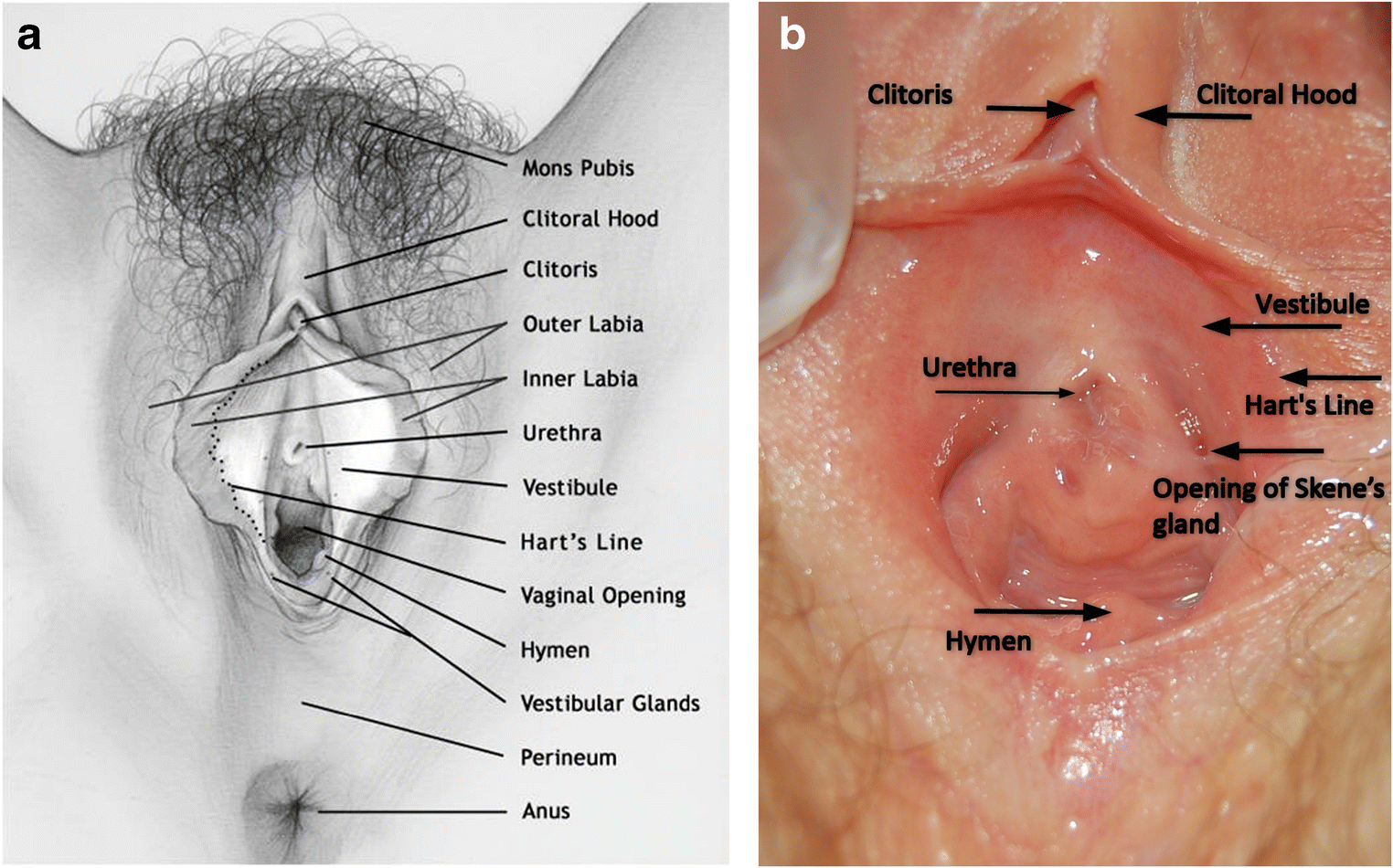
“Dyspareunia is defined as ‘recurrent genital pain associated with sexual intercourse’. Provoked vestibulodynia (PVD) is reported to be the most frequent subtype of dyspareunia in premenopausal women with a prevalence of 7% in the general population. Women with PVD typically experience a severe, sharp, burning pain upon vestibular touch or attempted vaginal entry. It is diagnosed through the cotton-swab test, which consists of the application of a cotton swab to various areas of the vulvar vestibule and surrounding tissue” (2).
Dyspareunia can be with touch around the vestibule, upon entry due to hypertonicity or hypotonicity of the pelvic floor muscles, with deep penetration that depends on the coital position, or pain that comes after sex or with orgasm.
What’s interesting about these two conditions is that it is very difficult to differentiate and diagnose properly. In reality, “vaginismus cannot be reliably differentiated from superficial dyspareunia” (2). The Journal of Psychosomatics Obstetrics and Gynecology suggest a multi-axial description of these syndromes, rather than having them separate.
What I want you to take away from this is that there are names/diagnoses that describe very similar experiences and sensations. And what’s great about both of these diagnoses is that they are TREATABLE. You don’t have to continue to experience this if your goal is to enjoy pain-free penetration during sex and overall healthy function of your pelvic floor. Because, let’s be honest, we know that consensual sex (mostly with orgasm) is very healthy for your pelvic floor AND your mind/soul when you can enjoy it.
How to Treat Pelvic Dysfunction
Through a trusting and open relationship with a physical therapist, some people find complete relief of both vaginismus and dyspareunia, which can include the following modalities:
Diaphragmatic breathing and relaxation techniques
Dilator protocol (during treatment and for home exercise program)
Manual therapy with down-regulation of the nervous system
Sensate focus touch protocol (embodiment exercises)
Address surrounding pelvic/lower body structures
Why Does Pelvic Floor Dysfunction Happen?
Why these syndromes even come about is a whole separate discussion and is always under research with variable results. The job of a physical therapist who understands the biopsychosocial model of treatment is to refer their patients who may be experiencing these symptoms due to psychological factors, attitudes about sex and sexual education, relationship factors, sexual abuse/trauma, or organic etiologies (“congenital abnormalities, infections, vestibulodynia, trauma associated with genital surgery or radiotherapy, vaginal atrophy, pelvic congestion, endometriosis, vaginal lesions and tumors, scars in the vagina from injury, childbirth or surgery, and irritation caused by douches, spermicides or latex in condoms”) (2).
In these cases, the following modalities can be utilized as a part of a treatment program:
Sex/marriage counselor/coach
Hypnotherapy
Lubricants and botox injections (MD/ND)
Somato-emotional release
How to Seek Out Help for Pelvic Floor Pain and Pain During Sex
These are just two out of many other sexual dysfunctions that can occur in womxn. If any of this sounds like you, know that you’re not alone. If you’re ready to address your issues, please reach out either to me or any pelvic floor physical therapist in your area so that we can get you started on this journey of self-discovery and empowered healing.
Message Dr. Brittney online today.
Crowley, T, Goldmeier, D, Wadsworth, J, Hiller, J. Clinical Review: Diagnosing and Managing Vaginismus. BMJ 2009;338:b2284.
Marie-Andrée Lahaie SCB. Vaginismus: A Review of the Literature on the Classification/Diagnosis, Etiology and Treatment - Marie-Andrée Lahaie, Stéphanie C Boyer, Rhonda Amsel, Samir Khalifé, Yitzchak M Binik, 2010. SAGE Journals. https://journals.sagepub.com/doi/full/10.2217/whe.10.46. Accessed January 17, 2021.
Zgueb, Y., Ouali, U., Achour, R., Jomli, R., & Nacef, F. (2019). Cultural aspects of vaginismus therapy: A case series of Arab-Muslim patients. The Cognitive Behaviour Therapist, 12, E3. doi:10.1017/S1754470X18000119